Abstract
Background
Von Willebrand factor (VWF) is an essential hemostatic protein and deficiencies of VWF predispose to mucocutaneous bleeding (MCB) such as seen in von Willebrand disease (VWD). VWD type 1 is characterized by incomplete penetrance and variable expressivity even in individuals and families with the same mutation in VWF . In addition to those patients with VWD type 1, there is a large subset of individuals that have VWF levels below 50 IU/dL, who suffer from MCB but do not meet the full criteria for VWD (VWF levels less than 30 IU/dL). The mechanisms for low VWF levels in these patients are poorly understood but are thought to be due to decreased synthesis and/or decreased secretion, increased clearance, or altered proteolysis. Endothelial colony forming cells (ECFCs, also known as blood outgrowth endothelial cells or endothelial progenitor cells) are a source of donor-specific endothelial cells and have demonstrated defects in VWF release and packaging in VWD. ECFCs have been previously studied in patients with VWD, but have not been evaluated in individuals with low VWF levels.
Hypothesis/Objective
We hypothesize that the study of ECFCs from individuals with low VWF levels will reveal deficiencies of abnormal VWF release and shed light on the mechanisms of low VWF.
Methods
ECFC Derivation: Patients with low VWF levels and MCB (30-50 IU/dL) were enrolled in a IRB-approved study and whole blood was collected into sodium heparin vacutainers, layered on Ficoll and centrifuged to isolate the mononuclear cell layer, which is then plated in a twelve-well collagen coated plate. After extended incubation, the presence of phenotypically ECFCs was confirmed by visual morphology and by single stain flow cytometry with appropriate (positive/negative) staining for the endothelial cells markers CD146, CD105, CD31 and negative non-endothelial cell markers CD34, CD90, CD133, and CD45.
Stimulated Release of VWF from ECFC: ECFCs were plated in 12 well tissue culture plates. For stimulated release, the cells were exposed to 1mL serum-free media ± phorbol-12-myristate-13-acetate (PMA) (50ng/mL) for 1 hour. The conditioned media samples were then collected and assayed via the VWF:Ag ELISA.
Enzyme-Linked ImmunoSorbant Assay (VWF:Ag ELISA): A 96-well plate was be coated with anti-VWF antibodies and after blocking and incubation with respective samples VWF levels were determined anti-VWF primary and HRP-linked secondary antibodies; values were compared to a standard curve and normalized to cell surface area. Results are analyzed via ANOVA with correction for multiple comparisons.
Results
ECFC Derivation: A total of seven ECFC lines were created, 5 from individuals with MCB and VWF levels between 30-50 IU/dL (4:1 female: male ratio, age range 11-54 years) and 2 from healthy controls (2 female, age range 22-39 years, control ECFC 1, control ECFC 2) without symptoms of MCB.
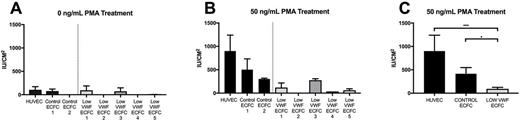
VWF release from patient derived endothelial cells: When treated with 0ng/mL of PMA, Low VWF derived ECFCs showed no demonstrable differences in VWF release into the conditioned media (Figure A). However, when treated with 50ng/mL of PMA, there is a noticeable trend of increased VWF release in the HUVEC and Control 1 and 2 ECFCs in comparison to the Low VWF ECFCs 1-5, although the results were not statistically significant (Figure B). When respective cohorts are grouped, the low VWF cohort demonstrates a statistically significant decrease in VWF at 50ng/mL as compared to HUVEC (p=0.0001) or control ECFC (p=0.0147) (Figure C).
Conclusions
We have demonstrated the ability to derive ECFCs from patients with Low VWF levels and MCB. Patient derived ECFCs from individuals with Low VWF levels demonstrate impairments in VWF release when stimulated with PMA and as a group, those individuals with low VWF levels demonstrate a significant decrease in VWF release. This decrease in stimulated VWF release is seen with several different individual patient samples and suggests that individuals with low VWF levels may have defects in VWF synthesis and or release that correspond to their lower plasma levels of VWF.
Ng: Shire: Consultancy; CSL Behring Heimburger Award: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal